Breathe Deep: What Air Pollution Tells Us About Asthma in New York City
In June 2023, smoke from Canadian wildfires turned New York City's skies orange. Though a striking visual of climate change for many, for vulnerable residents it was a serious health threat. Air pollution in NYC is not just an environmental issue, but a public health crisis shaped by climate and inequality. This study explores how six key pollutants relate to asthma hospitalizations across age groups, revealing how air quality reflects broader forces of climate, policy, and place.
New York City engulfed in smoke from Canadian Wildfires in June 2023
Image source: CNN, “Smog Is Choking New York. But for These Cities, It's Just Another Day,” June 8, 2023.
Air Quality and Public Health
Air pollution is well-established as a contributor to a wide range of public health risks, including respiratory illnesses and cardiovascular diseases. Research consistently demonstrates strong correlations between asthma and air pollutant exposure, while children, especially infants, are more vulnerable due to their still-developing lungs (Marmot & Bell, 2018). Fine particulate matter (PM₂.₅) and ozone are particularly dangerous, linked to asthma onset, emergency room visits, and worsened lung function (Bronte-Moreno et al., 2023; U.S. EPA, 2024).
In New York City, ozone has been shown to correlate with spikes in childhood asthma-related emergency room visits and hospitalizations (Sheffield et al., 2015), while both PM₂.₅ and ozone contribute to longer hospital stays for pediatric patients (Hardell et al., 2023). Although local policy efforts have led to a decline in PM₂.₅ concentrations, ozone-related health effects have remained persistent (Cohen et al., 2024).
Climate Change and Air Quality
As climate change accelerates, its role in shaping urban air quality has become increasingly apparent. Warmer daily temperatures catalyze reactions that increase the concentration of ozone and PM₂.₅ (Grigorieva and Lukyanets, 2021). Climate-driven wildfires—like the 2023 blazes that blanketed NYC—release black carbon and PM₂.₅ that travel across borders and linger in lungs (Tran et al., 2023).
Climate change also lengthens pollen seasons and increases allergen potency, contributing to respiratory conditions (West et al., 2023). As heat amplifies pollution and vice versa, a feedback loop emerges: warmer air produces more pollutants, which worsen air quality and reinforce warming. This self-reinforcing cycle underscores the urgency of addressing both climate change and air quality issues simultaneously (Grigorieva and Lukyanets, 2021).
Which Pollutants?
Our study looked at data on six air pollutants: PM₂.₅, black carbon, ozone, sulfur dioxide, nitric oxide, and nitrogen dioxide, all of which exacerbate respiratory health, with data provided by the New York City Environment & Health Data Portal. PM₂.₅ arises from vehicle emissions, fossil fuel combustion, and wildfire smoke. Black carbon stems from diesel engines and biomass burning. Ozone is a secondary pollutant, formed through heat-driven reactions in the atmosphere. The remaining gases—sulfur dioxide, nitric oxide, and nitrogen dioxide—are direct byproducts of fossil fuel combustion.
We then compared these pollutants to asthma hospitalization rates in three age groups: infants (0–4), children (5–17), and adults (18+), showing little explanatory power. For adults (Figure 1), there were weak linear trends but many outliers.
Figure 1. Individual Regression of Adult (18 and up) Asthma Hospitalization Rates for Different Air Pollutants
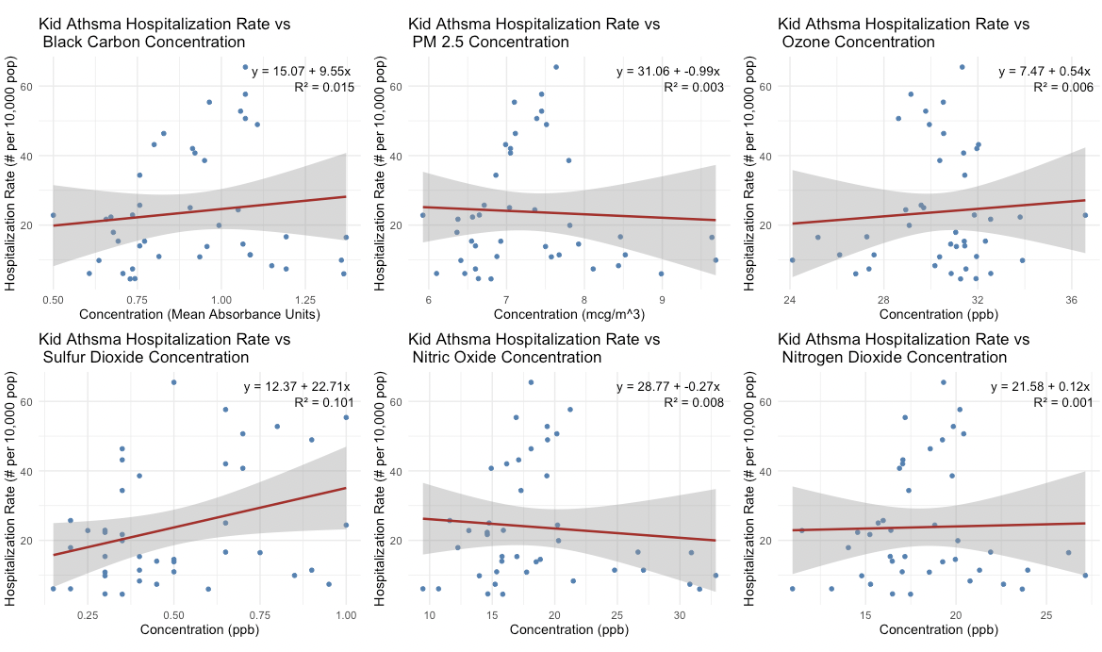
Similar results held for children (Figure 2) and infants (Figure 3), though the slopes were generally steeper for younger age groups, consistent with their biological vulnerability.
Figure 2. Individual Regression of Kid (5-17) Asthma Hospitalization Rates for Different Air Pollutants
Figure 3. Individual Regression of Infants (4 and below) Asthma Hospitalization Rates for Different Air Pollutants
Notably, we observed unexpected negative correlations across all age groups between PM₂.₅ and nitric oxide and asthma hospitalization rates—surprising in light of prior research linking both to increased respiratory risk.
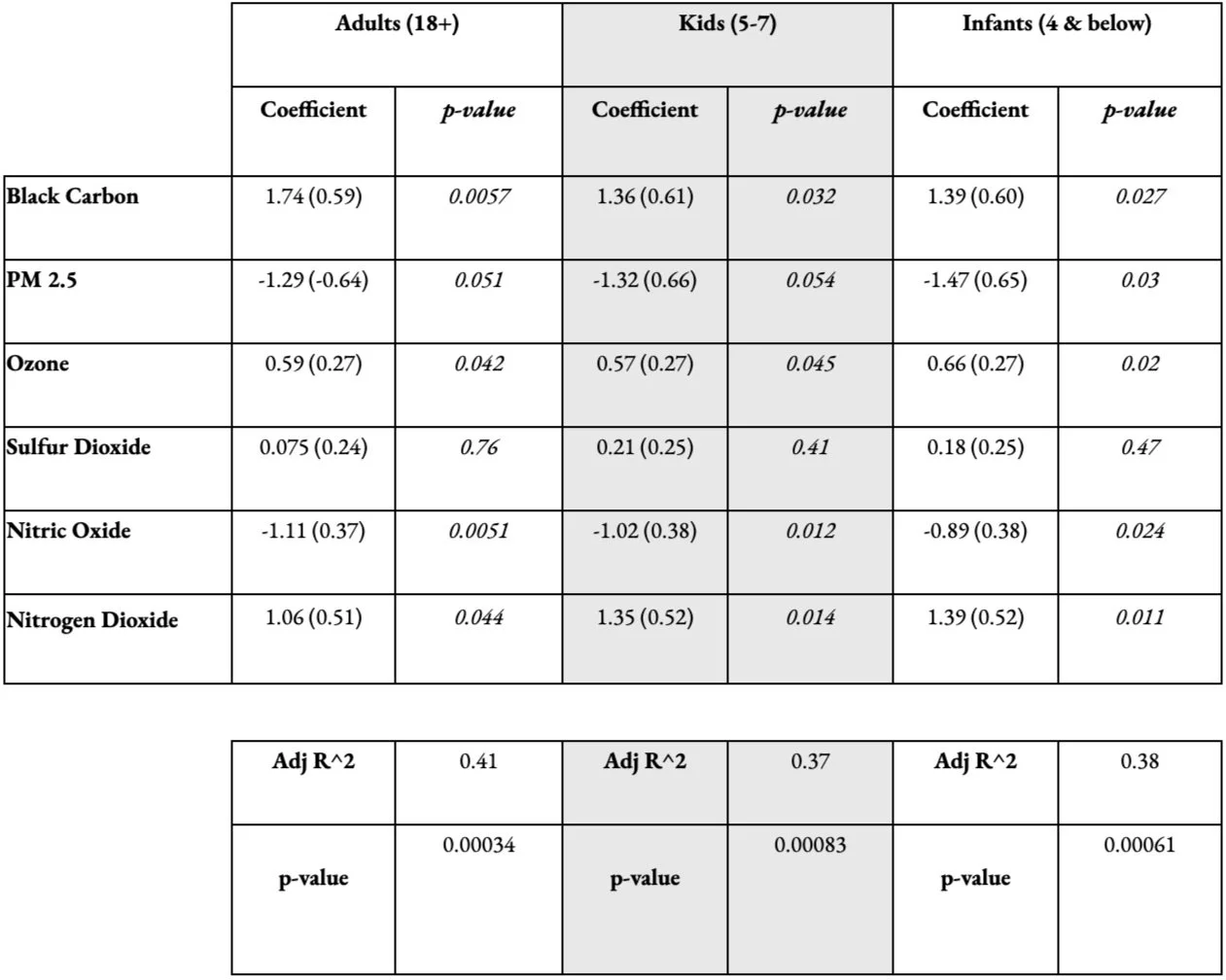
To probe deeper, we conducted a multiple regression analysis including all six pollutants. The standardized models, summarized in Figure 4, revealed consistent positive correlations between asthma hospitalizations and concentrations of black carbon, nitrogen dioxide, and ozone across all age groups. Even as climate change impacts worsen, it’s important to recognize the positive impact of local mitigation to reduce air pollutant concentrations (Lau et al., 2024). PM₂.₅ concentrations in particular have decreased citywide, possibly explaining the negative correlations in the regression models. The regression models suggest that pollutant interaction matters: it may not be one pollutant alone, but the cumulative presence of multiple pollutants, akin to a composite air quality index, that better predicts asthma hospitalization trends.
Figure 4. Multiple Regression Coefficients and P-values for Standardized Hospitalization Rates and Air Pollutants Across Different Age Groups
Compounding Impacts
As the climate crisis intensifies, its effects on human health grow more severe. Rising temperatures and extreme weather worsen air quality, increasing the risk of respiratory illness. Heatwaves can trigger dehydration and heat-related illness, while aggravating conditions like chronic obstructive pulmonary disease (Grigorieva and Lukyanets, 2021). Climate change thus compounds existing public health challenges.
Another critical dimension to consider is socio-cultural and economic stressors that increase exposure to pollutants. Poor air quality disproportionately impacts marginalized and underserved communities (West et al. 2023). The placement of industrial facilities, waste sites, and highways in racialized and lower-income neighborhoods leads to higher rates of asthma and respiratory illnesses, especially among children (Nishimura et al. 2013). The Bronx is a particularly vulnerable area, having the highest age-adjusted asthma death rates in New York State (DiNapoli 2014). In 2018, the establishment of a diesel trucking operation in the South Bronx raised additional concerns from residents about worsening air quality; by 2020, a 10-40% increase in truck and vehicle traffic was observed, as well as a 0.003 μg/m3 increase in black carbon (Shearston et al. 2020).
As climate change intensifies air quality and public health impacts, legislative solutions like the green amendment, which guarantees the right to clean air and water in the state constitution, are critical towards advancing environmental equity (Smith 2021). Recognizing these inequities contextualizes how air pollutants disproportionately affect respiratory health across various demographics in New York City.
All in all, our findings show that asthma risk in cities is shaped by more than individual pollutants, and instead by the cumulative impact of multiple pollutants, rising temperatures, and inequality. Considering the urgency of climate change, clean and equitable air must be a public health priority.
References
Bronte-Moreno, O., Gonzalez-Barcala, F.J., Munoz-Gall, X., Pueyo-Bastida, A., Ramos-Gonzalez, J., Urrutia-Landa, I. (2023) Impact of air pollution on asthma: A scoping review. Open Respiratory Archives, 5(2).
Cohen, A. S., Goldberg, R., Pitiranggon, M., Johnson, S., and Ito, K. (2024) Trends in risk from air pollution and attributable burden of asthma and cardiovascular morbidity in New York City. ISSE Conference Abstracts. https://doi.org/10.1289/isee.2024.061.
DiNapoli, Thomas P., (2014). The Prevalence and Cost of Asthma in New York State. New York State Comptroller. https://www.osc.ny.gov/files/reports/special-topics/pdf/health-asthma-2014.pdf
Grigorieva, E., and Lukyanets, A. (2021) Combined effect of hot weather and outdoor air pollution on respiratory health: Literature review. Atmosphere, 12(6). https://doi.org/10.3390/atmos12060790.
Hardell, J., Silver, E. J., Kavoura, I., Lee, D. S., and Gross, E. (2023). Childhood asthma in the Bronx, NY; the impact of pollutants on length of hospital stay. Journal of Asthma, 60(12), 2160-2169. https://doi.org/10.1080/02770903.2023.2225607.
Lau, K., Guo, J., Miao, Y., Ross, Z., Riley, K., Wang, S., Herbstman, J., and Perera, F. (2024). Major air pollution and climate policies in NYC and trends in NYC air quality 1998-2021. Frontiers in Public Health, 12. https://doi.org/10.3389/fpubh.2024.1474534.
Marmot, M., & Bell, R. (2018). The Sustainable Development Goals and Health Equity. Epidemiology, 29(1), 5–7. https://doi.org/10.1097/EDE.0000000000000773
Nishimura, K. K., Galanter, J. M., & Roth, L. A. (2013). Early-Life Air Pollution and Asthma Risk in Minority Children. American Journal of Respiratory and Critical Care Medicine, 188(3), 309-318. https://doi.org/10.1164/rccm.201302-0264OC
Shearston, J. A., Johnson, A. M., Domingo-Relloso, A., Kioumourtzoglou, M.-A., Hernández, D., Ross, J., Chillrud, S. N., & Hilpert, M. (2020). Opening a Large Delivery Service Warehouse in the South Bronx: Impacts on Traffic, Air Pollution, and Noise. International Journal of Environmental Research and Public Health, 17(9), 3208. https://doi.org/10.3390/ijerph17093208
Sheffield, P. E., Zhou, J., Shmool, J. L. C., Clougherty, J. E. (2015) Ambient ozone exposure and children’s acute asthma in New York City: A case-crossover analysis. Environmental Health, 14.
Smith, R. H. (2021, November 4). New York on track to pass environmental rights ballot proposal as voting changes get shot down. The City. https://www.thecity.nyc/2021/11/04/new-york-on-track-to-pass-environmental-rights-ballot-proposal-as-voting-changes-get-shot-down/
Tran, H. M., Tsai, F. J., Lee, Y. L., Chang, J. H., Chang, L. T., Chang, T. Y., Chung, K. F., Kuo, H. P., Lee, K. Y., Chuang, K. J., Chuang, H. C. (2023) The impact of air pollution on respiratory diseases in an era of climate change: A review of the current evidence. Science of The Total Environment, 898. https://doi.org/10.1016/j.scitotenv.2023.166340.
U.S. Environmental Protection Agency. (2024, June 20). Particle pollution and respiratory effects. https://www.epa.gov/pmcourse/particle-pollution-and-respiratory-effects
West, J.J., C.G. Nolte, M.L. Bell, A.M. Fiore, P.G. Georgopoulos, J.J. Hess, L.J. Mickley, S.M. O'Neill, J.R. Pierce, R.W. Pinder, S. Pusede, D.T. Shindell, and S.M. Wilson. (2023) Ch. 14. Air quality. Fifth National Climate Assessment. (Crimmins, A.R., C.W. Avery, D.R. Easterling, K.E. Kunkel, B.C. Stewart, and T.K. Maycock, eds). Washington, DC: U.S. Global Change Research Program. https://doi.org/10.7930/NCA5.2023.
This was a collaborative project by myself, and group members: Enzo Cremers, Olivia Gish, Siddharth Gundala, and Mirha Syed